
You will receive directions from the Quality Improvement Organization (QIO) regarding additional appeal options. We work to streamline the way we process claims. Medicare routes the appropriate claims to. You can file claims with us electronically or through the mail. The Quality Improvement Organization will respond to you as soon as possible, but no later than 14 days after receiving your request for a second review. Medicare uses the member eligibility file to verify any secondary insurance carrier.
Aetna corrected claim timely filing limit 2021 how to#
You may ask for this review immediately, but must ask within 60 days after the day the Quality Improvement Organization said no to your Level 1 Appeal. Timely Filing of Claim Submissions.120 Claims Processing Timeframes. how to wash a melin hat remington 1187 red dot mount. Within 48 hours the reviewers will tell you their decision. Ban of Advance Beneficiary Notice of Noncoverage (ABN) for Medicare Advantage (MA).
When you'll hear back from the Quality Improvement Organization (QIO) (Please refer to above directions regarding filing an expedited appeal) If you miss the deadline for contacting the Quality Improvement Organization about your appeal, you can make your appeal directly to us instead.
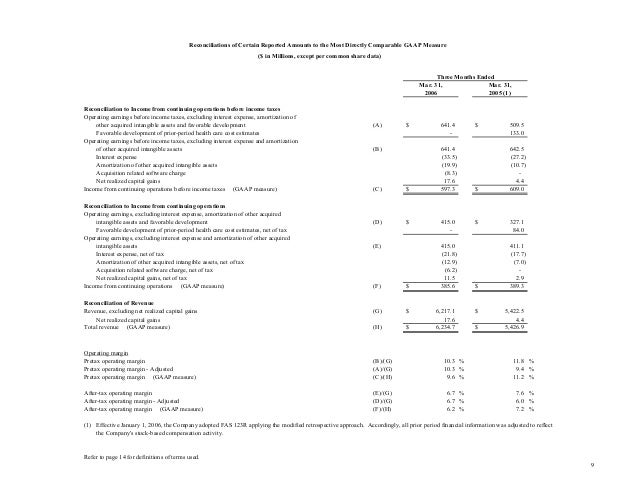
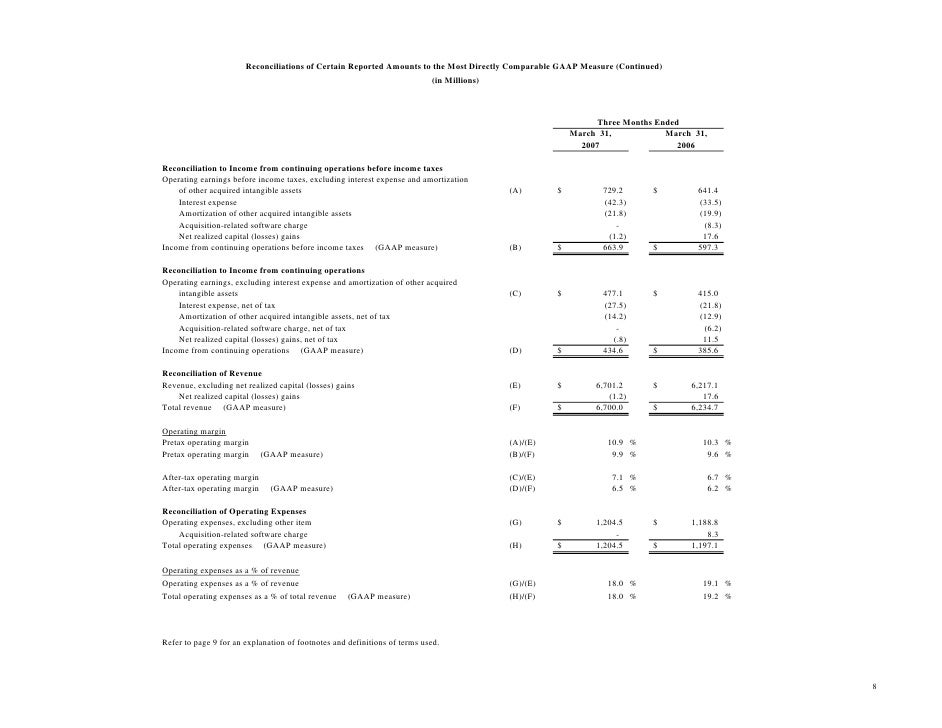
You must contact the Quality Improvement Organization to start your appeal no later than noon of the day after you receive the written notice telling you when we will stop covering your care. Claim Resubmission (Corrected Claim) a claim that is resubmitted to Aetna Better Health Premier Plan MMAI via the same process of a new day claim (via provider’s claims tool, Aetna’s claims portal. You can ask to change this decision so you're able to continue coverage. When your coverage for that care ends, we'll stop paying our share of the cost for your care. You’ll receive a "Notice of Medicare Non-Coverage (NOMNC)" in writing at least 2 days before we decide it’s time to stop covering your care. (Usually, this means you’re getting treatment for an illness or accident, or you're recovering from a major operation.)
Address, phone number and practice changes. SUMMARY OF CHANGES: Section 6404 of the Patient Protection and Affordable Care Act (the Affordable Care Act) reduced the maximum period for submission of all Medicare fee-for-service claims to no more than 12 months, or 1 calendar year, after the date of service. Skilled nursing care as a patient in a skilled nursing facility Find forms and applications for health care professionals and patients, all in one place.You have the right to keep getting your covered services for as long as the care is needed to diagnose and treat your illness or injury if you’re getting:


 0 kommentar(er)
0 kommentar(er)
